After a short break – I am back. And grateful. So far, I got around 5,000 visits on the three previous chapters, 100 times more than an average peer-reviewed paper, and exactly 5,000 more than expected.
Your interest and trust allow me to use this opportunity to talk in a few paragraphs about the other side of the coin. About a rarely discussed issue.
A problem
The global scene. In 2018, we celebrated the 40th birthday of Louise Brown; and that of our science. On this occasion, special pages were published in leading journals. Fertility and Sterility invited 66 prominent scientists, pioneers of a given field, who overviewed their specific area, using frequently phrases like “the most important advance”, “improved dramatically”, “the most comprehensive development” “tremendous” etc., on 140 pages. Almost all papers were optimistic and happy with past achievements, outlining bright perspectives for the future.
No intention to question any of these statements. I just missed one reference among the 643 cited. That of Gleicher, published in the same journal the previous year. Its statements were explained in detail two years later in an open-access journal (Gleicher et al., Worldwide decline of IVF birth rates and its probable causes, HRO 1-7, 2019, doi:10.1093/hropen/hoz017). Please let me insert the figure showing the US annual birth rates following fresh autologous IVF cycles from 1995 to 2016.
Comments are accessible in the paper, here I just want to provide the fact.
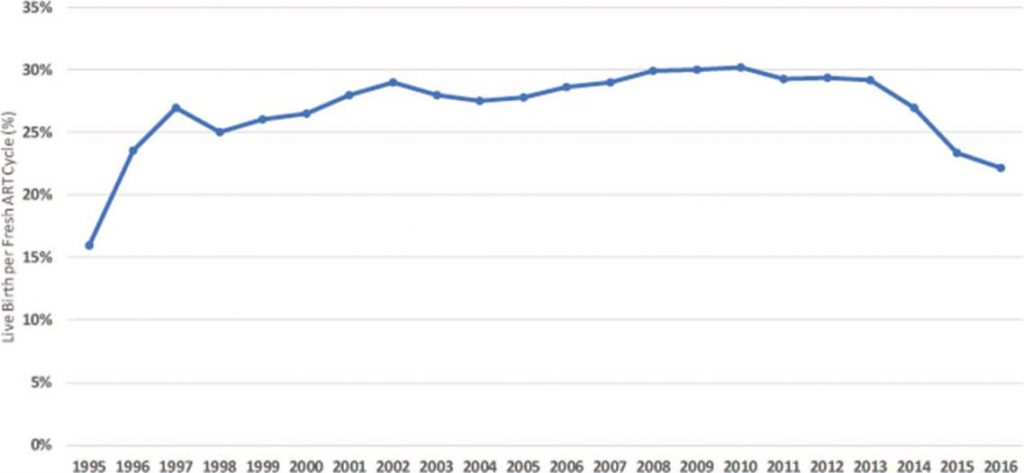
Fig. 1: Annual birth rates in the USA following fresh autologous IVF cycles from 1995 to 2016.
Another issue, now from England. In January 2020, the popular newspaper Daily Mail has published the worst and best success rates of IVF clinics in England. The difference in live birth/started cycle rates was 3.6-fold (12 vs. 43%). The two clinics were located just a 50-minute drive away. According to the statistics of the Human Fertilisation and Embryology Authority, none of these results was strikingly different from the others, results of the remaining 77 clinics were evenly distributed on the efficiency scale.
And, are you aware of the fact that with the current capacity we can only treat 1 out of 55 infertile couples of the world? And even with a 10% yearly increase (that is far above the current realities), it may take 30 years to be able to help just 30% of those who need it (Vajta et al., 2015)?
Embryology is part of it. A less known, and probably less important, still interesting fact. Rare, but not at all unique situation. Two respected European clinics have published results in the same year (2017) about two versions of an embryo culture system. No difference in media composition and amount, embryos, incubation. Everything was the same – except for the outcome. Could not be more different. Not slightly. Shockingly different between the two labs. Just the contrary. No explanation. A big question mark.
(I will not give more details here, those interested can get the references in a private letter.)
Such issues may create concerns and doubts. This was an experiment. What will happen to the patients? What to do, who to trust, how to proceed? I may also mention the single medium – two-phase medium – single medium detours. Just to mention, in cattle IVF we survived the whole period (from 1996, up till today) by using for seven days (!) a single medium ( Holm et al. 1999), a close analogue to those broadly advertised in human IVF today.
Then the list of temporarily fashionable add-ons: assisted hatching with various techniques, blastocoel collapse, artificial oocyte activation, sperm DNA fragmentation, IMSI, PICSI, PGT-A (maiden name PGS), dry incubators, embryo glue, and even timelapse – all with questionable value on the overall outcome. It was not me who said so. All doubts supported by comprehensive and systematic reviews.
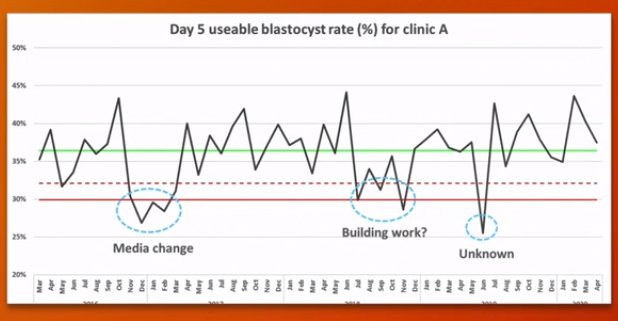
But, we also find problems in our own lab. Methods that work perfectly elsewhere just fail to produce the expected results in our settings, for months, sometimes for years. Even more annoyingly, an established technique or work phase just collapses, results become unacceptable, and remain so, despite our best efforts. These so-called “problem periods” are more common than supposed. (see the pre-conference lecture of Dean Morbeck: The IVF lab in 2030, ESHRE 2020;
In an experimental lab, scientists can freely turn to the wide community of colleagues worldwide for help. In a domestic animal lab, we still may have several good friends around for advice. However, in a human IVF lab, codes, rules, bosses and commercial interests restrict open discussions. In most cases, we can only use our own – more or less limited – resources and experiences in the given issue, with possible delays in finding the right solution.
So, we have a big problem here and it is our duty to find a solution.
Let us start with the weakest link of the chain that keeps us paralysed.

Technology transfer
By digging deeper we have to realize that one of the biggest obstacles hampering advancement in embryo labs is the lack of established ways for technology transfer. The most obvious example is that of vitrification. A seemingly simple, rather primitive manual procedure. Everybody can learn and perform it in a few hours, maximum one day. Then, why do I meet dozens of versions of my OPS technology worldwide, deviating from the original method and compromising seriously the outcome? Why does it require several months to reach the acceptable efficiency, and why are still considerable differences between laboratories even after years of continuous application?
Firstly, vitrification is not as simple as it seems to be. There are many small issues, traps and tricks that need attention to learn, and practice to overcome. Just like driving a manual car.
Secondly, you have no licensed driving schools and official exams with strict requirements. You have no police that detects your strange driving and punishes your inappropriate actions with a fine, disqualification or even prison. Well, you may say, driving is dangerous and human lives are at risk.
And with vitrification?
I do not want to send armed policemen in each IVF lab – but I miss very much the appropriate training.
Right now, the possibilities are restricted to:
- distributors, who (apart from the rare exception) have very superficial training in the given issue and very limited time to deal with you,
- exhibitions, where everybody focuses on coffee, meal and presents,
- conference lectures, the purpose of which is to create interest, not to teach
- workshops, that are both short and overcrowded, mostly social events,
- manuals, that are either too short, or too long, both hampering to focus on important details
- videos on youtube that are superficial and linear, with no chance to feedback
- a few weeks’ visit in a lab where the technology is run on the highest level
a great opportunity, but the privilege of a few lucky people
- chain teaching, between people with a modest knowledge in the topics;
My personal visits as a consultant were more or less successful, but required at least a week in a given unit, and repeated online consultation afterwards. Most clinics could not afford the time and effort, and my possibilities were also limited.
After frustrating experiences, we tried something different, by using the unexploited possibility offered by the last decade -
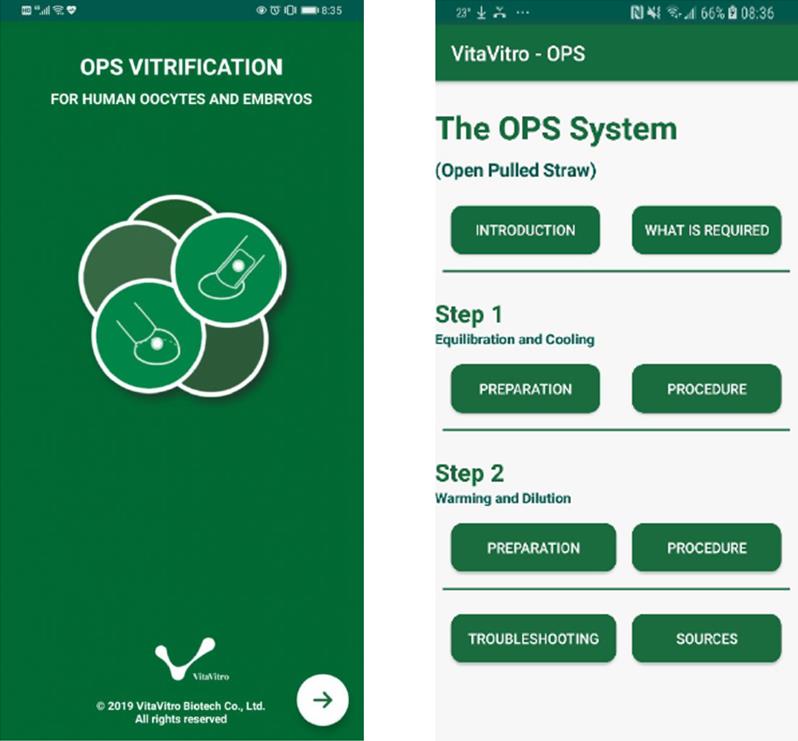
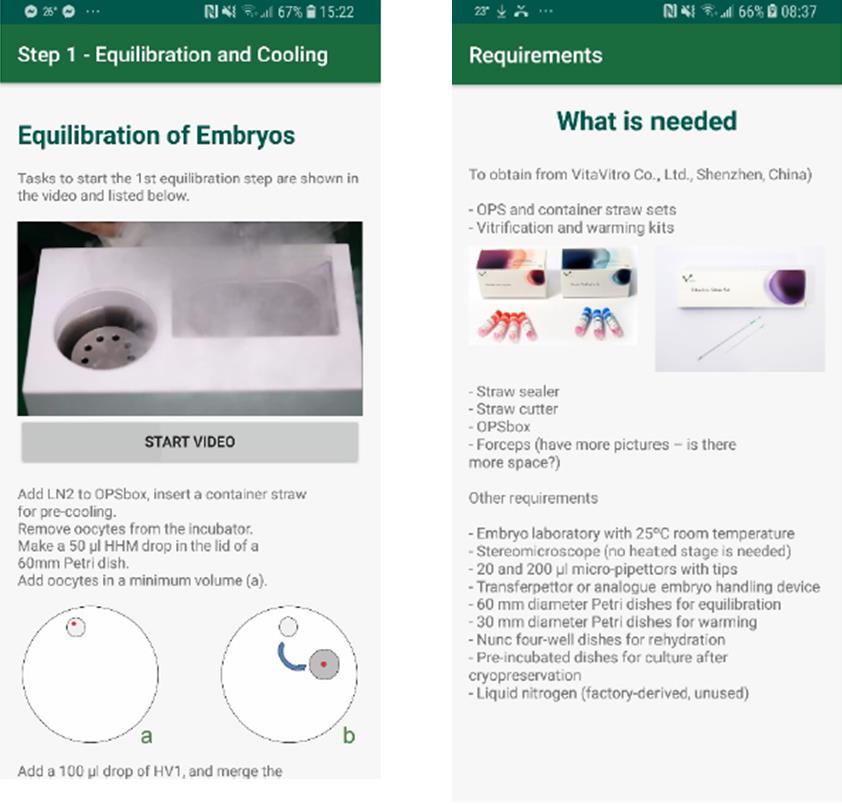
a mobile app that is not a manual, not a video, not a guide, but A COACH providing
- step-by-step, on-time instructions during the whole vitrification-warming process,
with a built-in stopwatch function
-interactive, personalized information
with options to choose the appropriate route
- ample possibility to obtain background information,
opinions and suggestions,
- direct contact to the inventor and producer.
Here is the first (public) version of the OPSapp.
hyperlink+QR Code android hyperlink+ QR Code iOS
At this point, however, we need more resources.

Please let us know your opinion about the idea in general (to make coaching apps for embryology lab procedures) and specifically about the OPSapp.
All suggestions will be considered and answered; the best ones will be placed on this webpage and followed in our future projects.
Just tell us, how could it be better. Thanks, mates.
Contact us:
Email: tech@vitavitro.com
Webpage: www.vitavitro.com/contact/
or on my Linkedin post for Chapter 4.

